Appealing underpayments is one of the most routine, and painful, parts of the revenue cycle. If you’ve worked an appeal, you’ve felt it. Your team spends hours rebuilding the same arguments, rewriting the same language, and reformatting the same documents over and over again. The process is slow, highly manual, and frustrating. Inconsistencies in how appeals are written can directly affect how quickly your team recovers the money you’ve owed.
And yet, when appeals are well structured, they work. Clear, policy-backed appeal letters lead to faster payer responses, cleaner reprocessing, and more predictable outcomes.
Sometimes the challenge is knowing where to start. A denied or underpaid claim sits in front of you, and you’re left staring at a blank page, unsure how to structure the appeal when every payer plays by slightly different rules.
This blog breaks down the core elements of an effective appeal letter, shows you what payers look for during review, and helps you bring more consistency and clarity to your appeals - without starting from scratch.
The core structure of effective appeal letter
Payers receive thousands of appeals every week. The ones that move through review quickly tend to follow a consistent pattern. These elements matter the most to many payers:
1. Start with claim details up front
List everything a reviewer needs without making them hunt for it. This reduces follow-up requests and helps accelerate review.
- Provider name
- Provider TIN
- Provider NPI
- Member name
- Member ID #
- Member date of birth
- Claim number
- CPT codes and modifiers
- Date(s) of service
- Rendering facility
2. State the purpose clearly
This can be as simple as:
- RE: Request for Corrected Reimbursement
- RE: Request for Reconsideration
A direct headline immediately sets the tone and makes the intent of the letter clear.
3. Present the basis for the appeal
This is where the substance lives. The strongest appeals:
- Cite CMS or MFPFS rules
- Reference payer-specific policies
- Explain why the original payment determination conflicts with these rules
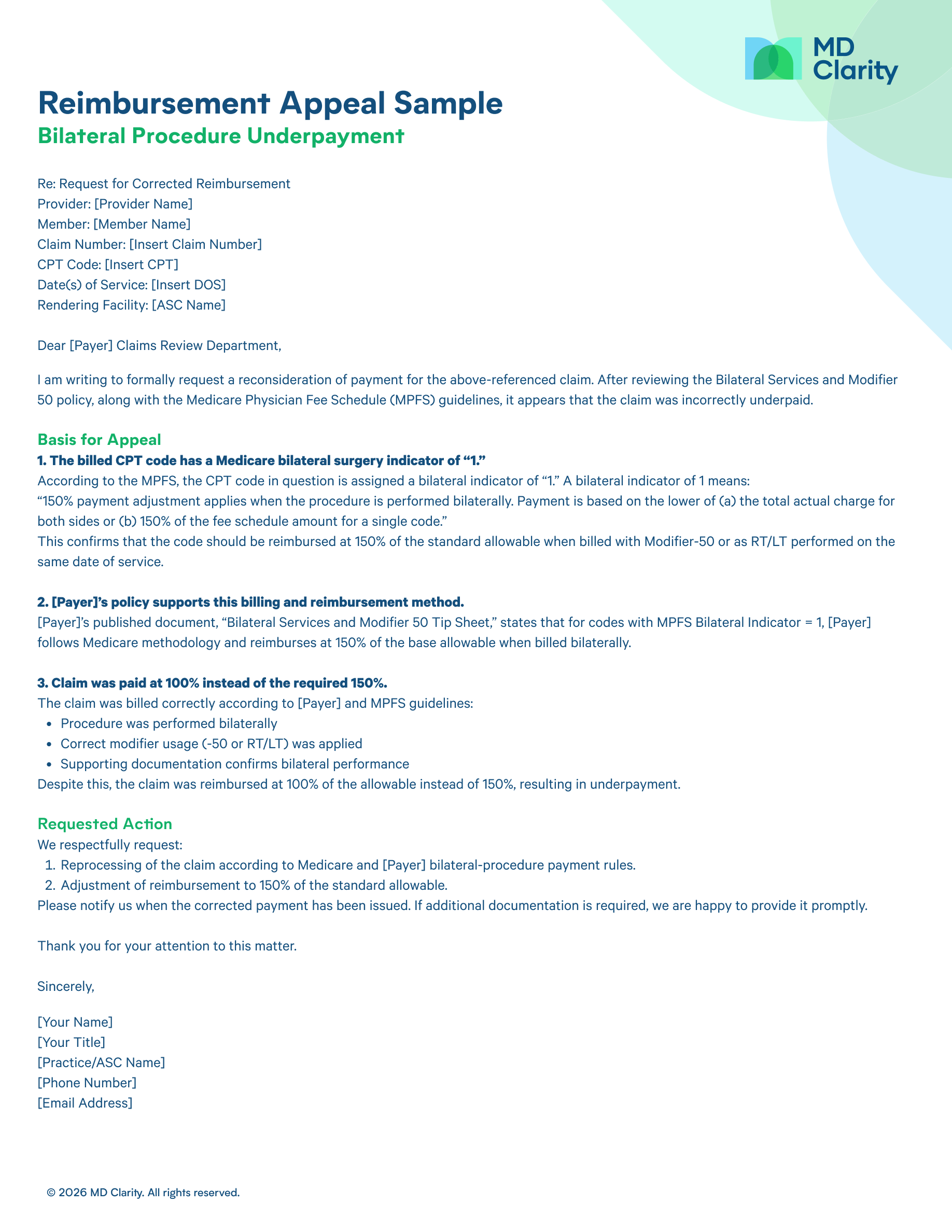
In the example above, the appeal:
- Used the MPFS bilateral indicator to show the correct reimbursement methodology
- Pointed to the payer’s own bilateral services policy to reinforce the argument
- Clearly explained that the claim was billed correctly but paid at 100% instead of 150%
The result is an argument that’s factual, policy-based, and easy for a reviewer to verify.
4. Explain the payment error
Be simple and direct.
- What was paid
- What should have been paid
- Why
Stick to the facts and avoid unnecessary narrative.
5. Specify the action needed
State exactly what you want the payer to do:
- Reprocess the claim
- Adjust the allowable
- Apply the correct reimbursement percentage
- Correct the code edit
When the requested action is clear, reviewers can move forward without making assumptions.
6. Close professionally
Offer to provide additional documentation and include clear contact information. This helps close the loop quickly and avoids delays.
Why a Well-Structured Appeal Works
A strong appeal is built on logic, clarity, and policy support. The bilateral underpayment example illustrates why it worked:
- Cited the MPDFS bilateral indicator to establish the correct reimbursement methodology
- Referenced the payer’s published policy confirming alignment with Medicare rules
- Demonstrated correct billing and modifier usage
- Clearly stated what was paid versus what should have been paid
- Made a precise request for claim to be reprocessed at 150%
Making strong appeals repeatable
Most teams know how to write a strong appeal. The issue is scale. When every denial or underpayment means rebuilding an appeal from scratch, the process becomes cumbersome. Hours are lost to repetitive work, quality varies from one team member to the next, and key details slip through the cracks. Even with a solid argument, the manual effort required to pull everything together becomes a bottleneck that delays recovery.
To make strong appeals repeatable, teams need structure and not workarounds. That starts with templates designed around what payers expect to see, not generic letters.That means templates built around what payers expect, claim details pulled in automatically, and easy access to the data and policies that support each appeal. When those pieces are in place, appeals stop being one-off tasks and become a faster, more reliable part of the revenue cycle.
How MD Clarity helps team build better appeals faster
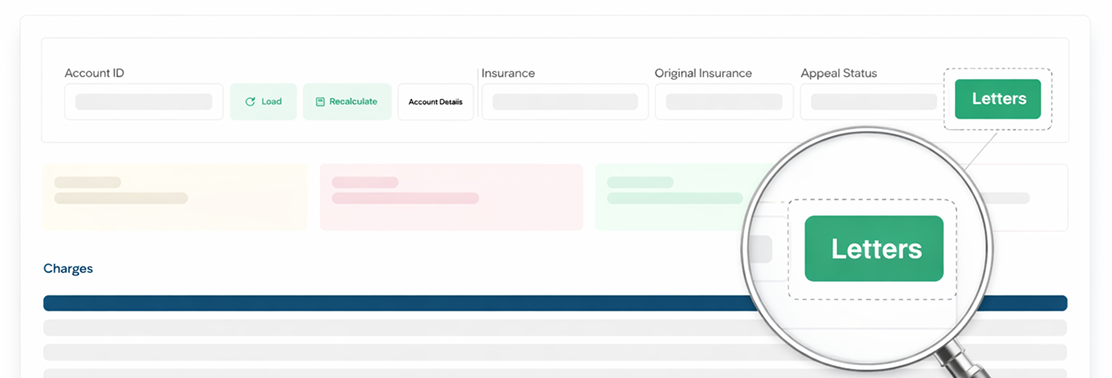
Instead of digging through claims data or rebuilding language from scratch, teams can start with pre-generated, claim-aware appeal letters that are already structured around what payers expect.
With the Appeal Letters feature, teams get:
- Claim-specific fields auto-filled from existing account data
- A structured appeal format proven to work across payers
- Consistent language that eliminates staff-by-staff variation
- Templates aligned with payer expectations from clarity and completeness
- Appeal letters ready to download and send
The tool pulls in the relevant information automatically and offers templates that teams can use as-is or tailor to their workflows, making it easier to stay consistent while saving time.
If you’d like to learn more, connect with a member of our Customer Success team for a deeper walkthrough on how to set everything up for your organization.
And if you haven’t already, join our community forum, where providers and revenue cycle experts ask real appeal questions, share what’s working, and help each other solve issues that don’t always fit neatly into a blog post.
FAQs
Get paid in full by bringing clarity to your revenue cycle


.svg)
.svg)