What's New and What It Means For You
We’re cutting out scavenger hunts and guesswork so your teams can move faster with fewer surprises. With letters that build themselves and insight tools that make payer conversations data-driven, you can spend less time stitching together context and clearly connect what happened to what happens next.
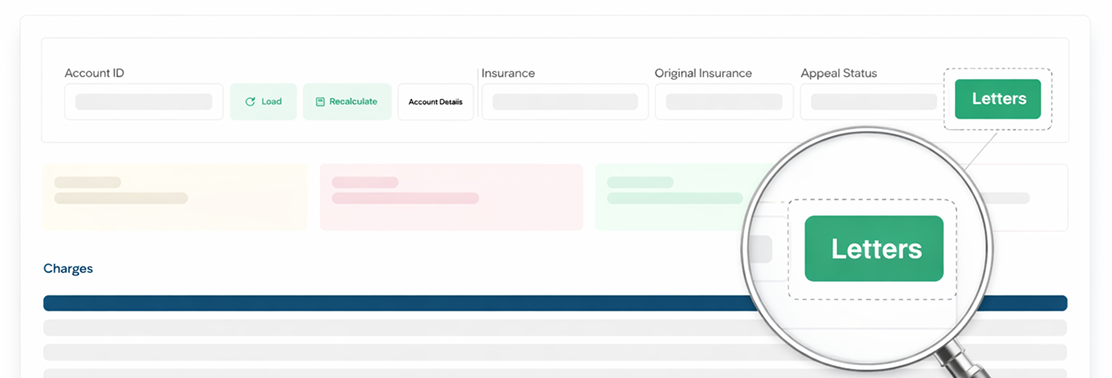
Appeal Letters
Generate polished, evidence-backed appeal letters directly from MD Clarity—no copying, pasting, or rebuilding templates. The system pulls denial data, payer details, and contract language to create a ready-to-send letter in minutes.
- Accelerate recovery with automatically pre-populated, claim specific letters
- Improve consistency with standardized language and formatting
- Reduce manual effort so teams can focus on high-value accounts
How to Access: Available in Account view top-right corner labeled Letters. If you need template customizations, contact your Customer Success Manager.
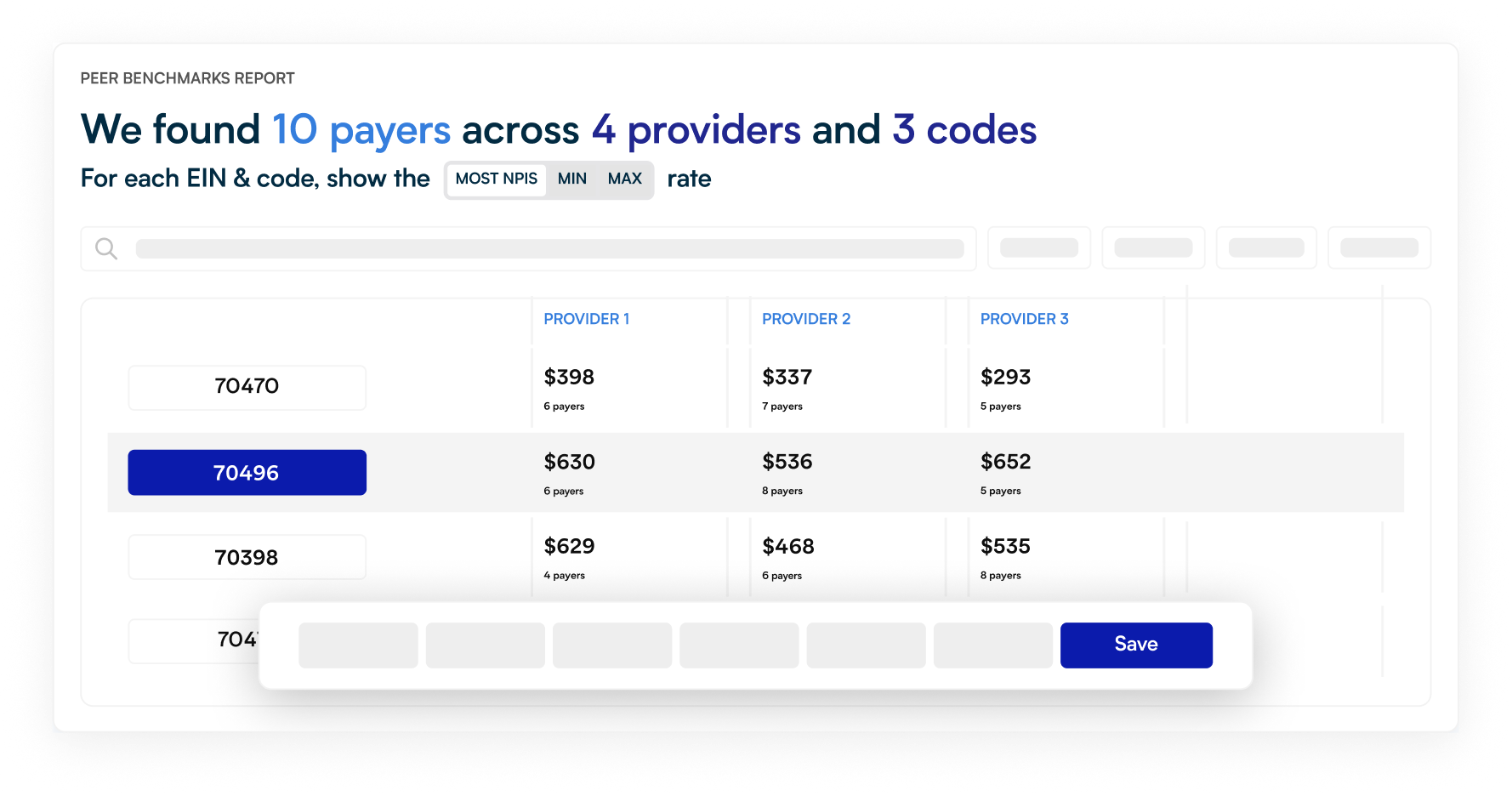
Payer Benchmarking
Negotiating without market intelligence leaves money on the table. Payer Benchmarking gives you the data you need to strengthen renewals, prioritize payer strategy, and evaluate growth opportunities with confidence.
- Identify gaps in service-line performance relative to peers
- Strengthen negotiation positions with clear market comparisons
- Evaluate new markets and service lines with realistic expectations
How to Access: Available as an add-on through our partner portal. Contact your Customer Success Manager to enable access or schedule a walkthrough.
Visual Refresh & Workflow Enhancements
We’ve tightened core workflows and upgraded the estimator to automatically factor in a patient’s secondary insurance.
Enhancements to the Visit Page
- Redesigned visit page for clearer insurance and visit summaries
- Ability to reorder visit charges directly in the visit page
- More consistent workflows with corrected adjustments and updated notes capabilities
Secondary-Insurance Calculation Engine
- Automatic application of secondary benefits
- More accurate splits with improved sequestration + deductible modeling
- Stronger insurer mapping and full remittance visibility for better traceability
The refreshed UI is faster, clearer, and makes it easier to surface the right coverage details. Behind the scenes, improved eligibility parsing, sequestration handling, insurer mapping, and remittance visibility give the estimator cleaner, more complete data. With these logic upgrades, teams get far more accurate out-of-pocket estimates without extra steps and spend less time troubleshooting splits or rerunning calculations.
If you need help enabling any of these features or want a deeper walkthrough of what’s new, reach out to your MD Clarity Customer Success Manager or contact us. We’re here to make sure your teams get the full value from these updates and can put them to work right away.
FAQs
Get paid in full by bringing clarity to your revenue cycle


.svg)
.svg)


